Why Herniated Discs Need Decompression
Herniated discs can unsettle daily life, inciting sharp or radiating back pain, leg numbness, or even muscle weakness. Conventional options—like invasive surgery or heavy painkillers—carry drawbacks and lingering side effects. Spinal decompression therapy, by contrast, targets the mechanical root: gently expanding the vertebrae to reduce disc pressure and encourage natural realignment. Through a series of relaxed pull-and-release cycles on specialized equipment, herniated material retracts from nerve roots, sparing you constant discomfort. Coupled with rest, rehab exercises, and Dr. Elham’s integrative approach, decompression sessions can foster true disc healing, letting you enjoy normal pursuits again without fear of searing aches.
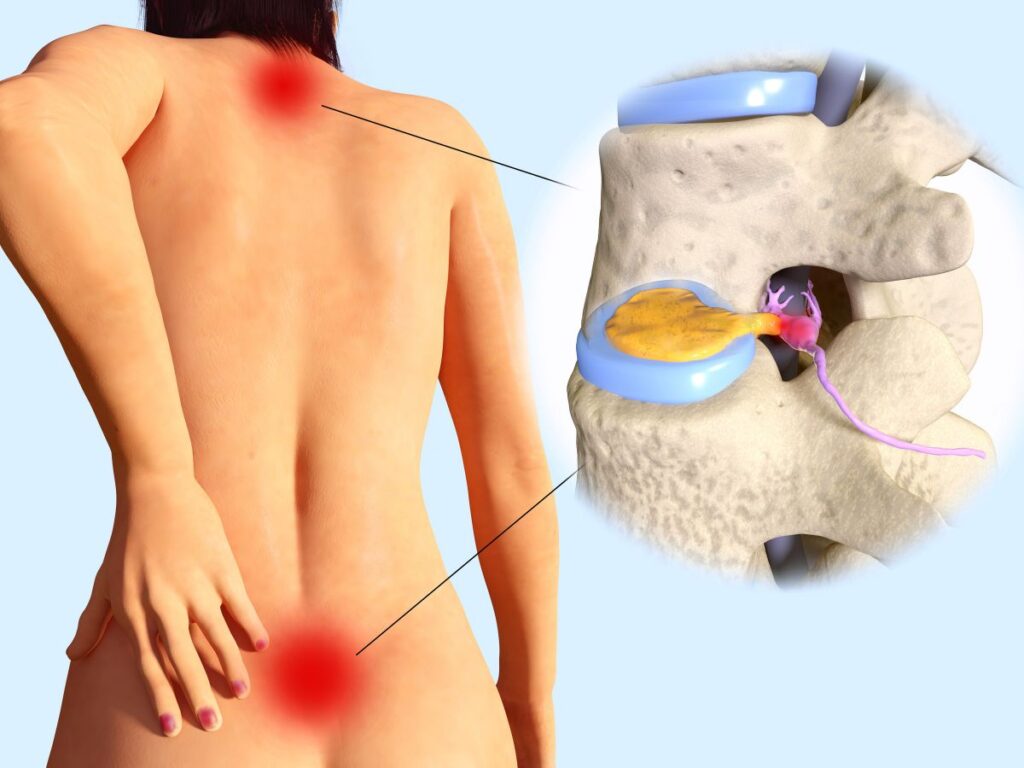
How Discs Become Herniated
Discs feature a tough outer ring and a jelly-like core, absorbing spinal shock. A sudden twist, heavy lifting with poor form, or gradual wear-and-tear can tear the outer layer, letting the gel protrude and press on nerve pathways. Sedentary habits, weak core muscles, and previous injuries heighten the risk. Once herniation irritates nerve roots, local inflammation and protective muscle spasms amplify pain. By applying controlled traction during spinal decompression, the therapy reduces the internal disc pressure—akin to briefly creating negative suction—so herniated material shifts inward. This mechanical relief contrasts starkly with quick symptom-masking, facilitating real structural repair.
The Mechanics of Decompression
Spinal decompression harnesses a motorized table or device that applies and releases gentle pulls along the spine. Patients lie comfortably, secured at the lower torso, as the machine rhythmically adjusts tension and relaxation phases. These cyclical stretches coax nutrient-rich fluids back into the disc, expediting healing. Dr. Elham customizes the angle and force for each patient’s unique disc location and severity, ensuring enough traction to decompress without aggravating tissues. Over multiple sessions—commonly 15 to 30—microtears mend, inflammation subsides, and the disc reestablishes its cushioning role without pressing on nerve routes.
Dr. Elham’s Whole-Body Perspective
While decompression focuses on the affected disc, Dr. Elham knows misaligned vertebrae or muscle imbalances can perpetuate disc stress. Thus, post-session chiropractic adjustments maintain proper spine alignment, encouraging discs to remain in their rightful place. He might incorporate targeted stretches or strengthening routines that fortify the core and ensure even weight distribution. For some, massage therapy relaxes tight back muscles that otherwise tug the vertebrae out of place again. This synergy fosters enduring progress, blocking small subluxations from unraveling the benefits of decompression and catapulting patients back to square one.
Benefits of Decompression for Herniated Discs
When integrated thoughtfully, spinal decompression can bring significant advantages:
- Relief from Nerve Compression: By expanding disc spaces, nerve roots escape chronic pinching and inflammation.
- Improved Disc Hydration: Intermittent traction draws fluids and nutrients into damaged tissues, speeding recovery.
- Avoidance of Surgery: Many patients bypass invasive procedures, reducing downtime and potential complications.
- Less Dependence on Medication: As pain abates naturally, heavy painkillers or muscle relaxants become optional.
- Greater Range of Motion: Freed nerves and relaxed muscles facilitate normal bending, twisting, or lifting once more.
Over time, these benefits reshape a herniated disc from a debilitating obstacle to a manageable condition, letting you re-engage with work, fitness, or family activities minus constant apprehension.
Preserving Gains After Decompression
Between sessions, self-care cements the disc’s healing. Dr. Elham may suggest core-strengthening exercises—like planks, bird dogs, or gentle back extensions—to stabilize spinal segments. Short walking or light stretching routines keep blood flowing, preventing stiffness from creeping in. Proper posture, particularly when seated, alleviates ongoing disc pressure, so adjusting chairs and desk height matters. Lifting heavy objects with correct form—bending at the knees, keeping the spine neutral—avoids re-straining the recovering disc. By integrating these small habits, you help the decompression outcomes stick, steering clear of re-injury or stubborn flare-ups.
Overcoming Daily Challenges
Herniated discs may cripple basic tasks, from rising out of bed to hoisting groceries. Decompression alleviates the nerve contact behind these stabs of pain or leg tingles, letting you approach each chore with less dread. Once inflamed tissues calm, Dr. Elham monitors how you move in everyday settings, offering micro-breaks or posture tweaks if you stand or sit extensively. Athletes can reintroduce training step by step, coupling traction benefits with mild strength-building. Over repeated sessions, the disc’s resilience amplifies, so routine motions—tying shoes, gardening—no longer risk a re-aggravation that throws life off track.
Potential Dangers of Unaddressed Herniation
Neglecting a protruding disc can pave the way for further disc degeneration or permanent nerve compromise. Chronic compression might weaken leg muscles, hamper coordination, or cause persistent numbness. The body could adopt skewed posture to dodge pain, building tension in other joints. Sleep and mood spiral as each day becomes a battle with stabs of discomfort. By contrast, spinal decompression quickly halts this cycle, tackling the mechanical root. Early and consistent therapy safeguards disc health, defending nerve integrity, and substantially cutting the chance of surgical interventions down the road.
A Glimpse of a Therapy Session
On arrival, Dr. Elham reviews pain changes and disc-related concerns. You’ll lie on a specialized decompression table, harnessed around the hips. The machine then gently tugs your lower body in cycles—expanding the vertebrae, then relaxing—adapting force to your comfort threshold. Some patients report a soothing stretch sensation in the spine. A typical session might span 15-30 minutes. Post-decompression, Dr. Elham performs a quick chiropractic adjustment or suggests mild stretches, sealing alignment gains and mitigating any residual tightness. Many leave feeling a reduction in leg tingling or back stiffness, with a sense of relief that builds over ensuing visits.
Charting a Pain-Free Path
Spinal decompression therapy for herniated discs offers a careful but potent route to disc rejuvenation, minimizing nerve irritation without surgical disruption. Typically, 2-3 sessions a week over several weeks produce steady healing. As the disc rehydrates and nerve compression eases, daily tasks become bearable once more. Dr. Elham’s holistic approach—chiropractic alignments, muscle conditioning, posture education—ensures each traction session endures beyond the clinic walls. Over time, the disc stabilizes, letting you reclaim normal function and glean confidence that your spine can handle life’s movements minus the dread of recurring searing back pain.